Pancreatic Cancer
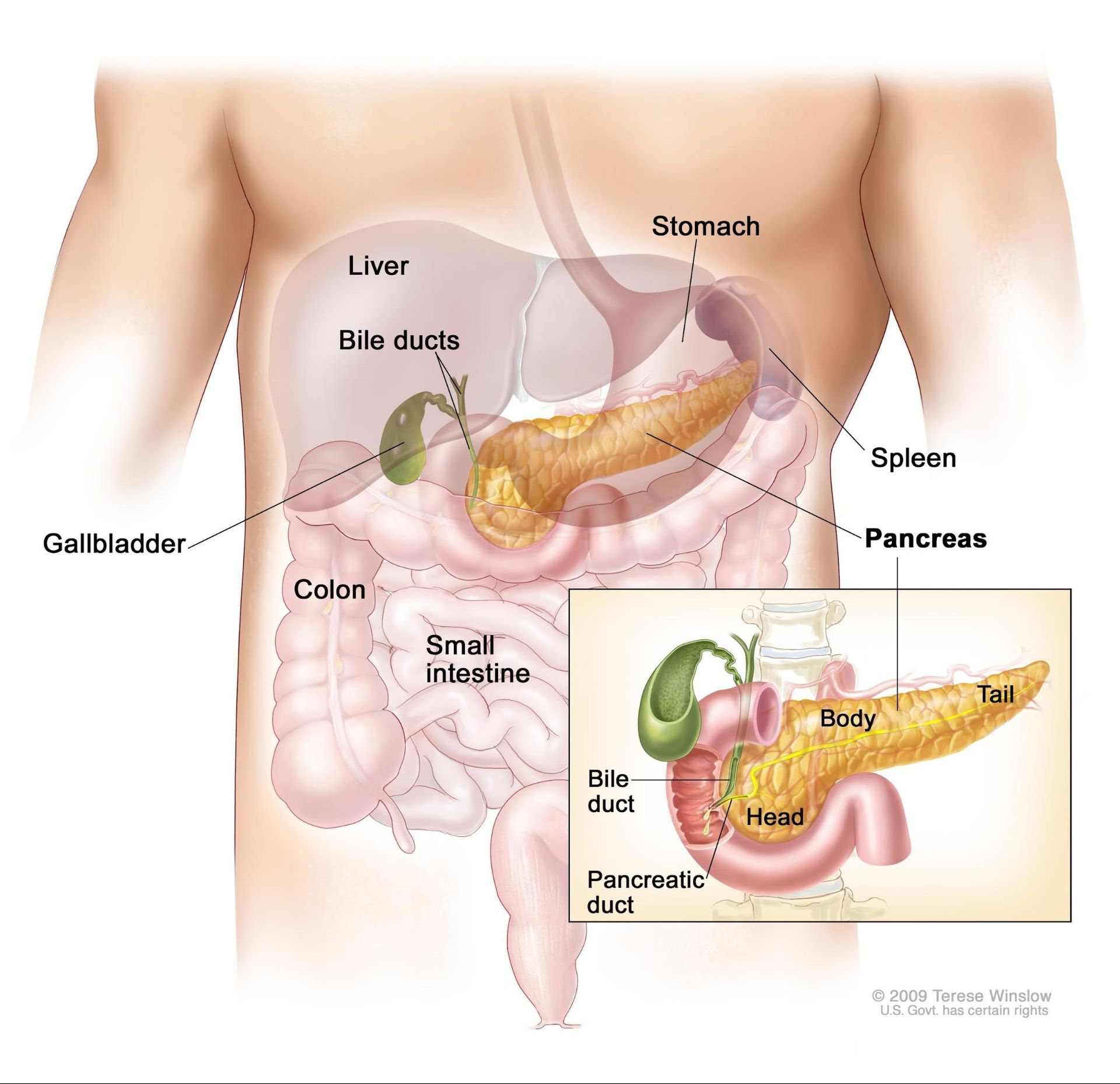
Where is our pancreas?
The pancreas is an organ that sits in the abdominal cavity behind the stomach.
What does your pancreas do?
The pancreas is part of the digestive and endocrine systems. It is a vital organ that helps regulate digestion and blood sugar.
Digestive System Function
It involves the secretion of digestive enzymes that aid the digestion and absorption of nutrients in the small intestine.
Endocrine System Function
It involves the production of several hormones, such as insulin, glucagon, somatostatin and pancreatic polypeptide.
What is Pancreatic Cancer?
Pancreatic cancer occurs when abnormal cells in the pancreas grow out of control and form a tumour. Pancreatic cancer has a particularly high mortality rate due to its aggressive nature. It is a significant concern because it can spread quickly and often has no symptoms until it has reached an advanced stage.
It is the 8th most common cancer in Australia and the 4th most common cause of cancer death (after lung and bowel cancer).
Impact of Pancreatic Cancer on Health
Some of the most common health problems associated with pancreatic cancer include:
- Digestive problems: Pancreatic cancer can interfere with the production of digestive enzymes, leading to problems with digestion and nutrient absorption. This can cause symptoms such as nausea, vomiting, and diarrhoea.
- Weight loss: Many people with pancreatic cancer experience unexplained weight loss, which can signify that the body is not getting the nutrients it needs.
- Pain: As the tumour grows, it can invade nearby organs, nerves and tissues, causing pain in the abdomen or back. In some cases, the pain can be severe and debilitating.
- Diabetes: The pancreas produces insulin, a hormone that helps to regulate blood sugar levels. If the tumour interferes with this function, it can lead to diabetes.
In addition to these health problems, pancreatic cancer can impact a person's emotional well-being. A diagnosis of pancreatic cancer can be frightening and overwhelming, and the treatment process can be challenging and demanding.
Types of Pancreatic Cancer
There are two primary types of pancreatic cancer:
- Exocrine pancreatic cancer: The most common type and occurs when the cells in the pancreatic ducts that produce digestive enzymes become cancerous. More than 95% of pancreatic cancers are classified as exocrine tumours. These tumours start in the exocrine cells, which make pancreatic enzymes that help with digestion. Within this category, the vast majority of tumours are adenocarcinomas.
- Endocrine pancreatic cancer: A much rarer type that affects the cells that produce hormones, such as insulin. Pancreatic neuroendocrine tumours are either functional (produce hormones) or nonfunctional (produce no hormones).
Who is Most at Risk for Pancreatic Cancer?
Pancreatic cancer can occur in anyone, but some people are at a higher risk than others. Some of the most significant risk factors for pancreatic cancer include age, smoking, obesity, a family history of pancreatic cancer, chronic pancreatitis, diabetes, chronic alcohol consumption, and certain genetic mutations.
Causes of Pancreatic Cancer
Despite the high mortality rate associated with pancreatic cancer, its causes are poorly understood.
Symptoms of Pancreatic Cancer
Pancreatic cancer symptoms depend on the site of the tumour within the pancreas and the degree of tumour involvement. There are few noticeable symptoms in the early stages of pancreatic cancer. As cancer grows, symptoms may include the following:
- Jaundice
- Light-coloured stools or dark urine
- Pain in the upper or middle abdomen and back
- Weight loss for no known reason
- Loss of appetite
- Fatigue
- Nausea
- Diarrhoea
- New onset diabetes
Stages of Pancreatic Cancer
Pancreatic cancer is classified into four stages based on the extent of the tumour and the spread of cancerous cells, with higher numbers indicating more advanced cancer. The stages are as follows:
- Stage 1: The cancer is confined to the pancreas and has not spread to nearby lymph nodes or other organs.
- Stage 2: Cancer has spread to nearby lymph nodes but not other organs.
- Stage 3: Cancer has spread to nearby blood vessels or organs but has not spread to distant organs.
- Stage 4: Cancer has spread to other organs in the body.
Staging helps doctors determine the appropriate treatment options and predict the prognosis for patients with pancreatic cancer.
Pancreatic Cancer Diagnosis
Pancreatic cancer is difficult to detect and diagnose for the following reasons:
- There are no noticeable signs or symptoms in the early stages of pancreatic cancer.
- The signs of pancreatic cancer mimic many other illnesses.
Diagnosing pancreatic cancer typically involves a combination of imaging tests, blood tests, and biopsy. Imaging tests such as CT scans, MRIs, and ultrasounds are used to identify any abnormalities in the pancreas. Blood tests may be done to detect the levels of certain proteins that may indicate the presence of pancreatic cancer. Finally, a biopsy with endoscopic ultrasound may be necessary to confirm the diagnosis by analysing a sample of abnormal pancreatic tissue.
Tumour Markers
No tumour-specific markers exist for pancreatic cancer. Markers such as serum cancer antigen (CA) 19-9 have low specificity. Most patients with pancreatic cancer will have an elevated CA 19-9 at diagnosis. Over time, an increase in CA 19-9 levels may identify patients with progressive tumour growth. However, a normal CA 19-9 does not preclude cancer or recurrence. It's important to note that tumour marker levels can be influenced by various factors, including other medical conditions, so elevated levels of these markers do not always indicate the presence of pancreatic cancer.
Pancreatic Cancer Treatments
Treating pancreatic cancer depends on several factors, including the cancer stage, the tumour's location, and the patient's overall health. Some common treatment options include:
- Surgery: May remove the tumour if it is confined to the pancreas and has not spread to nearby organs or blood vessels.
- Radiation therapy: Uses high-energy radiation to kill cancer cells and shrink tumours.
- Chemotherapy: Uses drugs to kill cancer cells and prevent them from multiplying.
- Targeted therapy: Involves drugs that target specific proteins or other factors that promote cancer growth.
Surgical resection is the mainstay of curative treatment for pancreatic cancer. It provides a survival benefit in patients with small, localised pancreatic tumours. Patients with unresectable, metastatic, or recurrent diseases are unlikely to benefit from surgical resection.
Pancreatic Cancer Surgery
One of the most common treatments for pancreatic cancer is surgery, which involves removing the tumour and any surrounding tissue that may be affected by cancer.
Preparation for Pancreatic Cancer Surgery
Preparing for pancreatic cancer surgery involves several steps to ensure you are in the best possible condition before the operation. Here are some things to keep in mind:
- Quit smoking
- Follow a healthy diet
- Stay physically active
- Arrange for post-operative care, and most importantly
- Engage a healthcare provider as part of an integrated supportive care plan that includes dieticians, pain management, palliative, spiritual, and psychological support.
Pancreatic Cancer Post-Operative Care Plan
A post-operative care plan is essential to recover successfully after pancreatic cancer surgery. Here are some things to include in your care plan:
- Follow-up appointments: Attending all follow-up appointments with your doctor is essential to monitoring your progress and ensuring proper healing.
- Pain management: Your doctor will provide pain medication to manage any discomfort you experience during recovery.
- Incision care: Keep the surgical incision clean and dry to prevent infection. Your doctor will provide instructions on how to care for the incision.
- Diet: Your doctor may recommend a specific diet after surgery to promote healing and ensure adequate nutrition.
- Physical activity: Your doctor will instruct you on when you can resume physical activity and what types of activity are appropriate.
Life Changes After Pancreatic Cancer Surgery
Patients who have undergone pancreas cancer surgery may become diabetic. They sometimes require pancreatic enzyme supplements to help with digestion. They may also require medication to reduce acid secretion in the stomach.
Following surgery, some patients receive further treatment through chemotherapy or radiotherapy. Patients are followed over time to detect the recurrence of cancer. If the cancer recurs, treatment goals change from trying to achieve a cure to improving quality of life.
Treatment for the reduction of symptoms may be achieved with various conventional therapies.
Palliative measures that can improve quality of life while not affecting the overall survival rate include the following:
- Surgical or radiologic biliary decompression (ERCP)
- Relief of gastric outlet obstruction
- Pain control (EUS-guided celiac plexus block)
- Psychological care addresses the potentially disabling psychological events associated with diagnosing and treating pancreatic cancer
Pancreatic Cancer Prognosis
The primary factors that influence prognosis are:
- Whether the tumour is localised and can be removed entirely.
- Whether the tumour has spread to lymph nodes or elsewhere.
Exocrine pancreatic cancer is often not curable and has a poor overall survival rate. The highest cure rate occurs if the tumour is truly localised to the pancreas. However, this stage of the disease accounts for only 20% of cases.
Patients with localised disease and small cancers (<2 cm) with no lymph node metastases and no extension beyond the capsule of the pancreas have the best chance of long-term survival if they undergo surgery.
What if Pancreatic Cancer is Left Untreated?
If pancreatic cancer is left untreated, it can have severe consequences. As the tumour grows, it can spread to nearby organs and blood vessels, causing significant pain and discomfort. Cancer spreading to other parts of the body can lead to many symptoms, including bone pain, weight loss, and jaundice.
In some cases, untreated pancreatic cancer can lead to complications such as:
- Obstruction of the bile duct or pancreatic duct
- Infection in the bile duct
- Liver failure
- Blood clots